The Critical Insights into Ventricular Tachycardia (VT)
-p-1080.png)
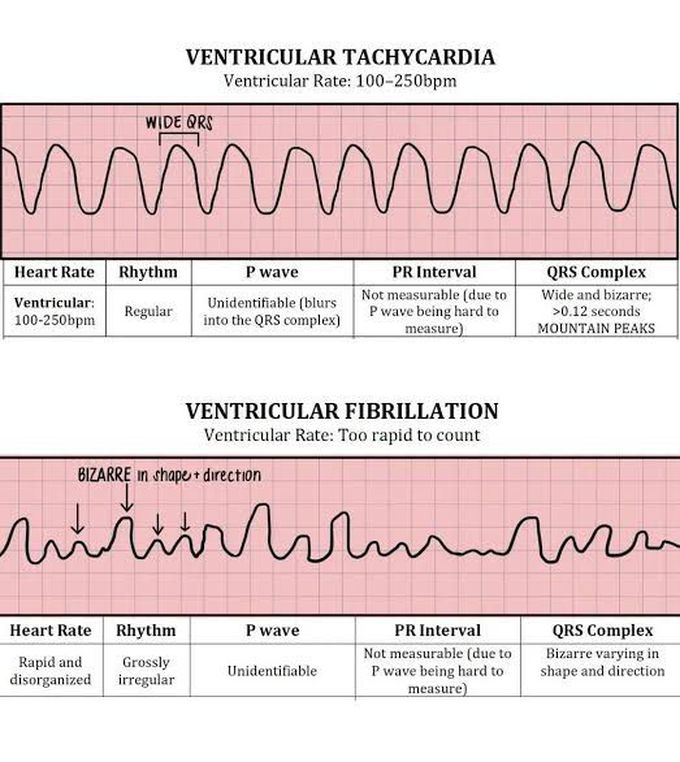
Ventricular Tachycardia (VT) is a serious heart condition that demands immediate attention due to its potential to escalate into life-threatening ventricular fibrillation. This article delves into the intricate details of VT, its types, causes, clinical presentation, and management strategies.
Understanding the Types of VT
VT is categorized into two main types:
- Monomorphic VT: Often resulting from myocardial infarction, it is distinguished by a consistent QRS morphology on the ECG.
- Polymorphic VT: This type includes Torsade de Pointes, associated with a prolonged QT interval and varying QRS morphologies.
Causes of VT
The onset of VT can be triggered by several factors, including:
- Structural heart disease, particularly post-myocardial infarction.
- Electrolyte imbalances such as hypokalemia and hypomagnesemia.
- Drug toxicity, notably from digitalis.
- Congenital Long QT Syndrome, heart failure, and cardiomyopathies.
- Recent conversion from atrial fibrillation.
Clinical Presentation and Diagnosis
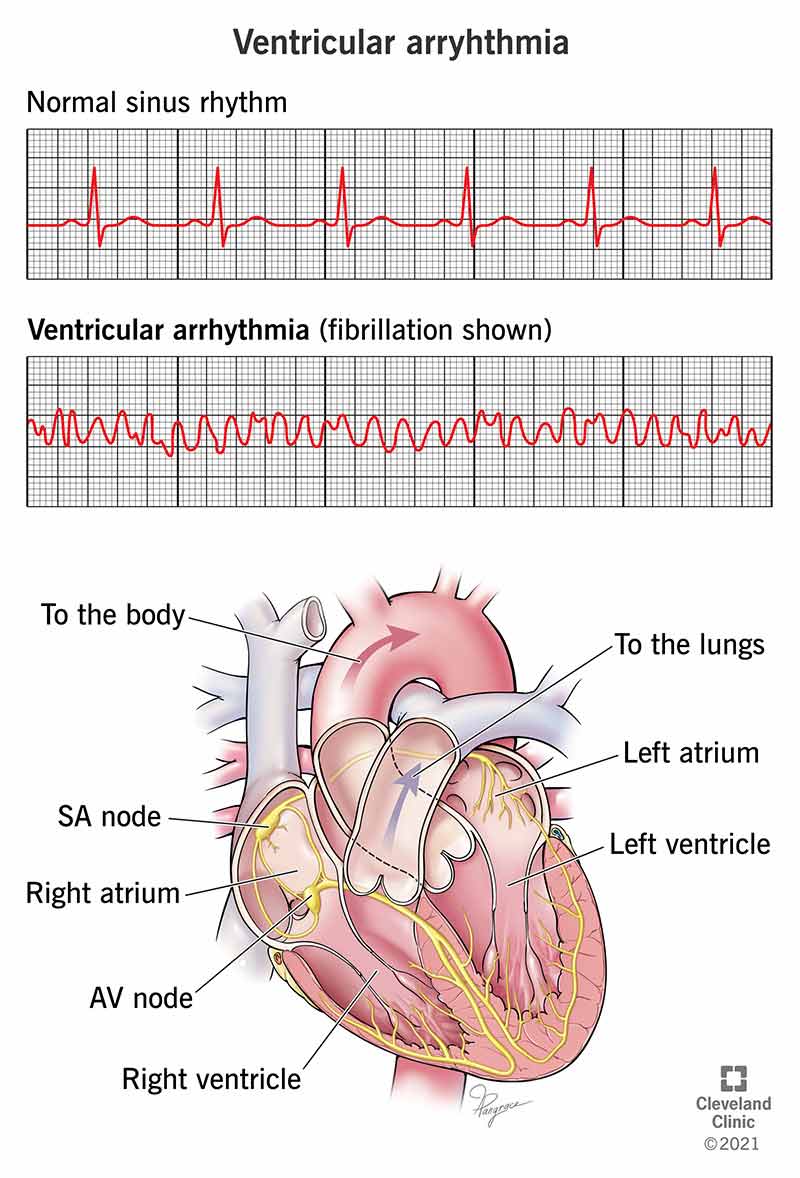
Patients with VT may experience symptoms ranging from palpitations and dizziness to syncope or cardiac arrest. Diagnosis is primarily made through ECG, showing broad-complex tachycardia.
Immediate Management Strategies
Effective management of VT includes:
- Synchronized Cardioversion: Recommended for patients presenting adverse signs like low systolic BP, chest pain, heart failure, or rapid heart rate.
- Drug Therapy: Options include Amiodarone, Lidocaine (used with caution in severe left ventricular impairment), and Procainamide.
- If drug therapy fails, further interventions such as an electrophysiological study or an implantable cardioverter-defibrillator (ICD) may be considered.
Special Considerations
It is crucial to avoid Verapamil in VT and address electrolyte imbalances promptly, particularly hypokalaemia and hypomagnesaemia. In some cases, severe hyperkalaemia can also precipitate VT.
Defibrillation Protocol
In line with the 2010 ALS guidelines, if a VF/pulseless VT arrest occurs in a monitored hospital setting, administer three quick successive shocks of 200 J, followed by immediate chest compressions with a 30:2 compression to ventilation ratio for 2 minutes.
The Role of Precordial Thump
A precordial thump might be effective if delivered within seconds of the onset of a shockable rhythm, though it should not delay other critical interventions.
Long-term Management and Prognosis
- ICD: Recommended for patients with recurrent VT or significant structural heart disease.
- Catheter Ablation: Considered for drug-refractory cases or non-ICD candidates.
- Beta-blockers: Beneficial in managing individuals with structural heart disease.
Preventive measures include monitoring and correcting electrolyte imbalances and avoiding medications that prolong the QT interval. The prognosis for VT patients has improved significantly due to advances in ICD technology and antiarrhythmic therapies, offering hope for better management and outcomes.
#VentricularTachycardia #VTInsights #CardiacHealth #HeartRhythm #MedicalResearch #Cardiology #HeartHealth #VTAwareness #Electrophysiology #Arrhythmia #CardiacCare #HeartCondition #VTDiagnosis #HealthEducation #HeartSpecialists
#HeartBeatDisorders #TachycardiaTreatment #CardiacScience #HeartRhythmDisorders #VTManagement #HeartElectrophysiology #CardiacArrhythmia #HeartDiseaseAwareness #VTRiskFactors #HeartHealthMatters #MedicalCardiology #VentricularArrhythmia #HeartConditionInsights #CardiacElectrophysiology #VentricularHealth

إرسال تعليق